Dehydration is a clinical condition resulting from insufficient body fluids, which may be due to insufficient fluid intake, excessive fluid loss, or both. Lack of fluids can affect the maintenance of the body's homeostasis and damage the normal function of tissues and organs. The human body is composed of approximately 60% water, which is necessary for normal blood circulation, metabolic processes, thermoregulation, and the functioning of the nervous system.
Dehydration reduces the amount of circulating fluid in the blood, which can cause a drop in blood pressure and an increase in blood clotting. It can cause heart and kidney failure and nervous system disorders. Dehydration can be mild, moderate, or severe, depending on the level of fluid loss, and may require different treatments. Severe dehydration can be fatal without treatment. Diagnosis of dehydration includes history taking, physical examination, and blood and urine tests. The mainstay of treatment is fluid supplementation, while prevention includes adequate fluid intake and adherence to a rational nutritional plan.
Dehydration and its causes
The causes of dehydration are multiple and complex, including both physiological and pathological factors.
Insufficient fluid intake: This is the simplest reason when a person does not consume enough water during the day, which may be due to unavailability, forgetfulness or special diets.
Increased fluid loss: This can happen during excessive sweating due to heat or intense exercise, frequent bowel movements, or vomiting.
Chronic diseases and conditions: Some diseases, such as diabetes, cystic fibrosis, or kidney failure, can increase the loss of fluid through urination or reduce the body's ability to absorb fluid.
Medicines and chemicals: Some medicines, such as diuretics or chemotherapy drugs, can promote dehydration by increasing the frequency of urination or causing vomiting and diarrhea.
Physiology of Adults and Seniors: Older people and young children are at greater risk due to physiological characteristics such as decreased thirst or increased sensitivity to heat.
Bad habits and diets: Drinking too much alcohol, caffeine, or following certain diets can cause or worsen dehydration.
Skin problems: Some skin conditions, such as burns or eczema, can increase sweating, causing dehydration.
Endocrine causes: Disorders that can affect the secretion of hormones that regulate water balance.
Trauma and surgery: Large fluid losses due to bleeding or loss of infusion fluids during surgery.
These causes show that dehydration can be multifactorial, and its prevention and treatment may require an individualized approach based on the specific cause, disease course, and patient needs.

What are the symptoms of dehydration?
Symptoms of dehydration are important in the diagnosis and treatment of this condition and can be classified as mild, moderate and severe.
1. Mild Symptoms:
Dry mouth and throat: This is one of the first and most common symptoms.
Increased thirst: The body tries to compensate for the lack of fluids.
Darker urine: Less fluid in the body often causes the urine to become darker in color.
Fatigue and dizziness: The following symptoms may occur due to reduced blood volume.
2. Moderate Symptoms:
Dry, cold skin: The skin may become more sensitive, cold, and feel clammy.
Decreased sweating: Less fluid can reduce the body's ability to cool itself through sweating.
Confusion and irritability: Dehydration can affect the brain, causing these symptoms.
Increased heart rate and breathing: Dehydration can increase the workload on the heart and lungs, making these organs less efficient.
3. Severe Symptoms:
Urinary frequency: Prolonged dehydration can lead to cessation of urine production.
Sagging skin and sunken facial features: Sagging skin can indicate severe dehydration.
Chills and heat: The body may lose its ability to regulate temperature.
Severe weakness or even loss of consciousness: This is a very serious symptom that requires immediate medical attention.
When diagnosing dehydration, doctors may also consider other parameters such as blood pressure, heart rate, and laboratory tests that may indicate fluid and electrolyte imbalances. It is important to understand that the symptoms of dehydration can vary according to age, health status and lifestyle, so an individualized approach and treatment are essential in the management of this condition.

How is dehydration treated?
Dehydration treatment is a complex process that depends on the degree of dehydration, the age of the patient, the state of health, as well as the underlying cause of dehydration.
Mild dehydration:
Oral rehydration: Mild dehydration can often be corrected simply by drinking more fluids, such as water, sports drinks, or special rehydration drinks with electrolytes.
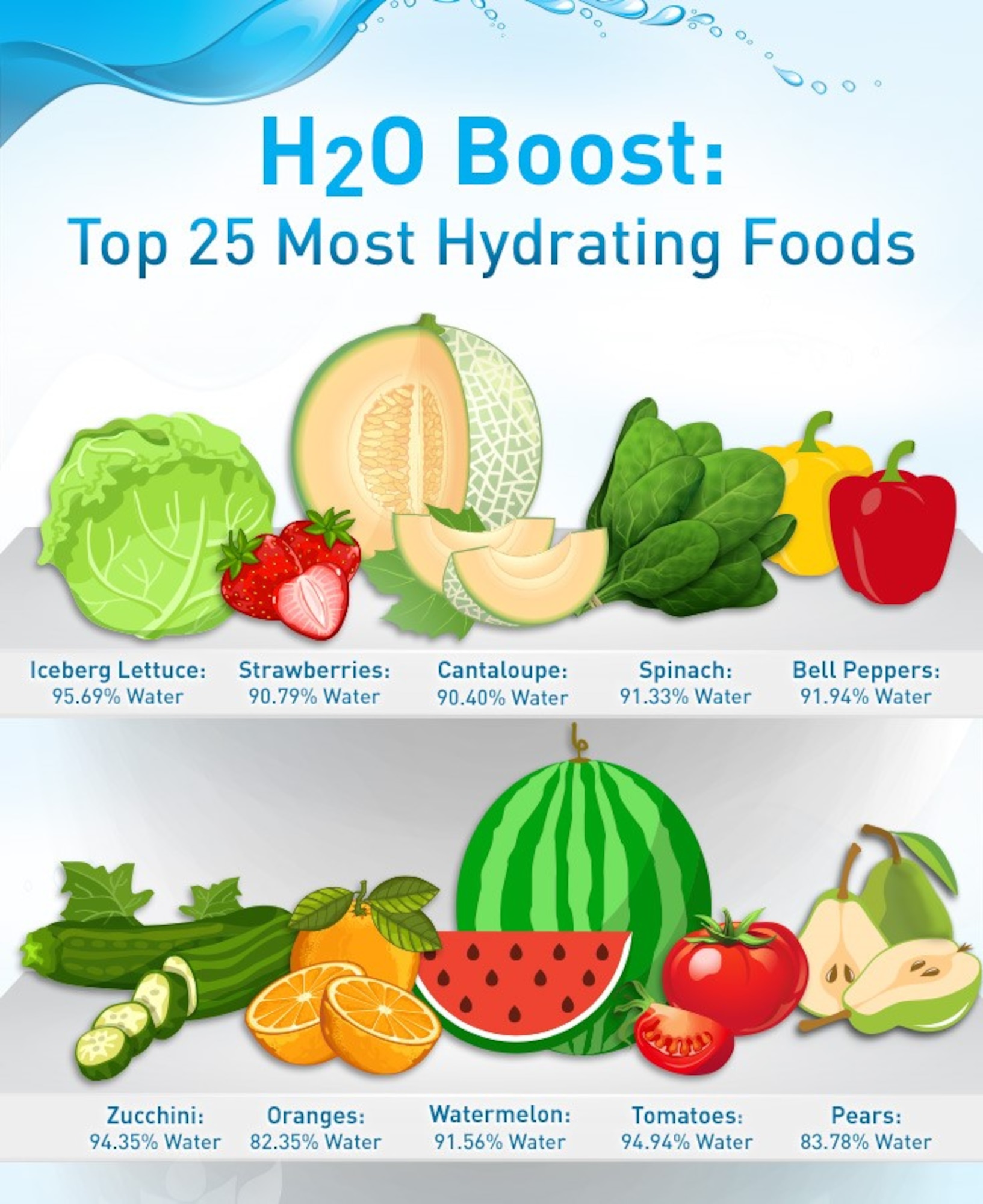
Diet: Eating foods with a high fluid content, such as fruits and vegetables, can also help.
Moderate dehydration:
Monitoring and supervision: In this case, medical supervision and monitoring may be necessary.
Infusion therapy: Some patients may need intravenous (IV) fluids to restore correct fluid and electrolyte levels.
Severe degree of dehydration:
Emergency hospital treatment: Severe dehydration is a life-threatening condition that requires immediate medical attention.
Intensive infusion therapy: IV fluids will be used to restore not only fluids, but also necessary electrolytes and nutrients.
Treating the underlying cause: Your doctor may also treat diseases or conditions that may have caused dehydration, such as diabetes or gastrointestinal disease.
Care and prevention
Education: Teaching about correct fluid intake, especially on a hot day or during sports.
Specialized drinks: Special rehydration drinks may be recommended for the elderly or those who have difficulty drinking enough fluids.
Individualized approach: The doctor can develop an individualized fluid intake plan based on the patient's age, weight and health status.
Treatment for dehydration is complex and must be performed by a qualified healthcare professional who can properly assess and treat the condition.
Dehydration prevention is an important and complex part of health care that involves more than just ensuring adequate fluid intake. It covers many aspects, such as choosing the right drinks and foods, individualized hydration plans, special care for certain medical conditions, and education about the risks and symptoms of dehydration.
Various factors such as age, physical activity, climatic conditions and health status can affect fluid requirements, so prevention of dehydration must be individualized and tailored to each individual. Maintaining fluid balance is an integral part of maintaining good health, and a competent and conscious approach to dehydration prevention can reduce the risk of complications and improve the quality of life.
Sources of information:
Mayo Clinic. (2018). Dehydration. Prieiga per https://www.mayoclinic.org/diseases-conditions/dehydration/symptoms-causes/syc-20354086
Cleveland Clinic. (2017). Dehydration and Heat Stroke. Prieiga per https://my.clevelandclinic.org/health/diseases/3927-dehydration--heat-stroke
Popkin, B.M., et al. (2010). Water, Hydration and Health. Nutrition Reviews, 68(8), 439-458.
Bennett, B.L., et al. (2013). Wilderness Medical Society practice guidelines for treatment of exercise-associated hyponatremia. Wilderness & Environmental Medicine, 24(3), 228-240.
Centers for Disease Control and Prevention (CDC). (2019). Get the Facts: Drinking Water and Intake. Prieiga per https://www.cdc.gov/nutrition/data-statistics/plain-water-the-healthier-choice.html
World Health Organization (WHO). (2005). The Treatment of diarrhoea: A manual for physicians and other senior health workers. Prieiga per https://apps.who.int/iris/handle/10665/43209
# dehidratacija