Sepsis is a serious and potentially fatal reaction of the body to an infection. It is a systemic inflammatory syndrome that occurs in response to an infection, usually caused by bacteria, but can also be caused by viruses, fungi or parasites. Sepsis causes a variety of pathological changes, including blood clotting and inflammation, which can lead to tissue damage, organ dysfunction and, in the most advanced cases, death.
The conditions of sepsis vary and depend on how strong and extensive the body's response to the infection is. Here are some conditions caused by sepsis:
Septic shock. This is the most serious form of sepsis, characterized by a drop in blood pressure despite fluid therapy. Septic shock can lead to organ failure and death.
Organ failure. Sepsis can cause temporary or long-term organ failure. These include kidney failure, heart failure, liver failure, and lung failure, including pneumonia and a syndrome called pulmonary distress.
Septic encephalopathy. This is brain damage caused by sepsis. This can manifest as confusion, lethargy, coma, or other neurological problems.
Blood circulation disorders. Sepsis can cause circulatory problems such as disseminated intravascular coagulation (DIC), which can lead to blood clots and bleeding.
Weakening of the immune system. Sepsis can have long-term effects on the immune system, increasing the risk of future infection.
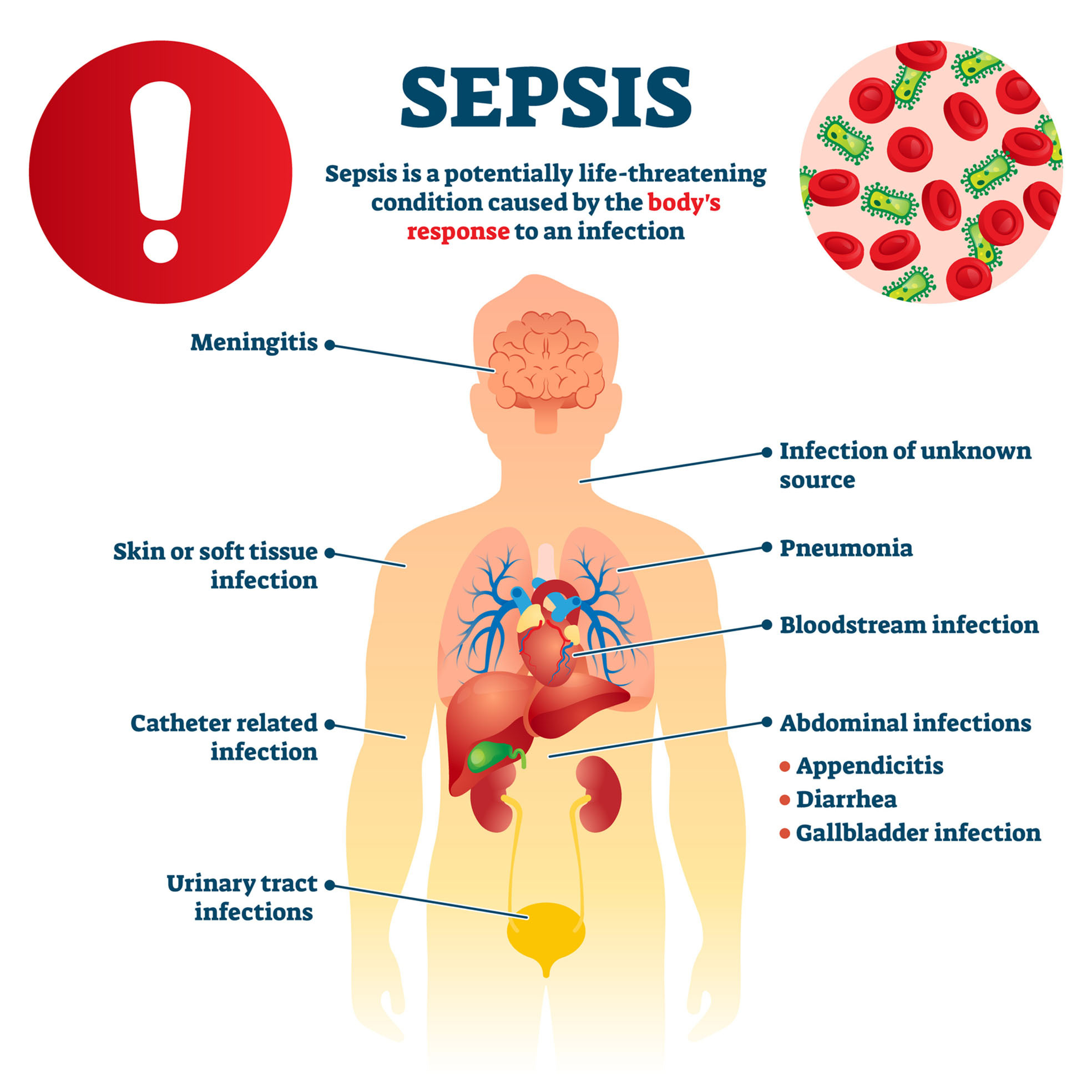
What causes sepsis?
Sepsis usually occurs in response to a bacterial infection, but can also be caused by other pathogens such as viruses, fungi, or parasites. The infection can start anywhere in the body, including the skin, lungs, kidneys, intestines, or urinary tract.
By its very nature, sepsis is a systemic response to infection in which the body produces inflammatory mediators to fight the infection. However, this response can be too powerful and uncontrolled, leading to inflammation throughout the body, which can lead to tissue and organ damage.
Risk factors that increase the likelihood of developing sepsis include: age (the elderly and children are more vulnerable), chronic diseases (for example, diabetes, AIDS, cancer), recent surgical or invasive medical procedures, diseases that weaken the immune system, and a recent injury or severe infection.
Symptoms of sepsis
Sepsis can cause a number of symptoms that depend on the location and severity of the infection. These symptoms may include:
High or low body temperature. During sepsis, the body temperature can rise above 38°C or drop below 36°C as the body tries to fight the infection.
Increased heart rate. Sepsis can cause tachycardia (increased heart rate), usually above 90 beats per minute.
Rapid breathing.
Confused state. Sepsis can cause confusion or other problems with brain function.
Edema or swelling. Sepsis can cause tissue swelling due to fluid build-up.
Unexplained weight loss.
Septic shock, the most severe form of sepsis, can cause the following additional symptoms:
Low blood pressure. Septic shock can cause hypotension (low blood pressure), characterized by a blood pressure less than 100 mmHg systolic.
Organ failure. Septic shock can lead to organ failure, including dysfunction of the heart, lungs, kidneys, liver, and brain.
Fatal condition. Without treatment, septic shock can be fatal.
How is sepsis diagnosed?
Sepsis is diagnosed based on clinical symptoms and laboratory tests. Clinical signs of sepsis may include high or low temperature, increased heart rate, rapid breathing, and confusion. In addition, doctors may perform certain laboratory tests, such as blood tests, to determine the presence of infection, organ function, and levels of inflammatory proteins.
When treating a patient who the doctor thinks has sepsis, it is important to start antibiotic therapy as soon as possible. Other treatments, such as intensive care or surgery, may also be needed to remove the source of infection.
Sepsis is a common medical condition worldwide that causes high mortality. The World Health Organization (WHO) has determined that sepsis causes about 6 million deaths worldwide each year. The number of sepsis is increasing, which can be explained by global aging, advances in medical technology that lead to more people living with chronic diseases, and the increasing resistance of bacteria and viruses to antibiotics.
Treatment
The goal of sepsis treatment is to control the infection, maintain organ function, and prevent complications. Treatment usually begins with emergency medical care, including blood tests and the use of antibiotics during the first few hours of treatment.
Antibiotics. Treatment begins with broad-spectrum antibiotics that work against many types of bacteria. After receiving accurate blood tests, doctors choose more specific antibiotics.
Vasopressors. If blood pressure does not rise after adequate fluid therapy, vasopressors, drugs that help raise blood pressure, may be used.
Oxygen and respiratory support. Many patients with sepsis may need supplemental oxygen or devices that help them breathe.
Surgery. In some cases, surgery may be required to remove the source of infection.
Supportive treatment. This may include medications, food and electrolytes by infusion, medicine to stabilize the heart rate or blood pressure, and other measures needed to maintain organ function and improve the patient's comfort.
Sepsis requires intensive treatment. Even with it, sepsis can lead to serious complications or death, so early diagnosis and treatment are critical.
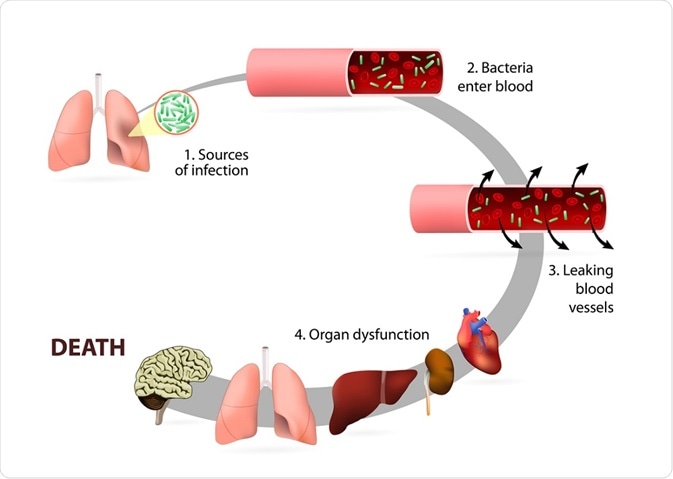
Sepsis is a dangerous condition caused by an infection that can rapidly progress to organ failure and death. Early diagnosis and treatment are vital because sepsis can progress rapidly. It is important to know the symptoms of sepsis and seek medical attention if they occur.
Sources of information:
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016.
Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003.
Angus DC, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001.
Martin GS. Sepsis, severe sepsis and septic shock: changes in incidence, pathogens and outcomes. Expert Rev Anti Infect Ther. 2012.
Bone RC, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992.
Mouncey PR, et al. Protocolised Management In Sepsis (ProMISe): a multicentre randomised controlled trial of the clinical effectiveness and cost-effectiveness of early, goal-directed, protocolised resuscitation for emerging septic shock. Health Technol Assess. 2015.
Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017.
# sepsis # infekcija






