
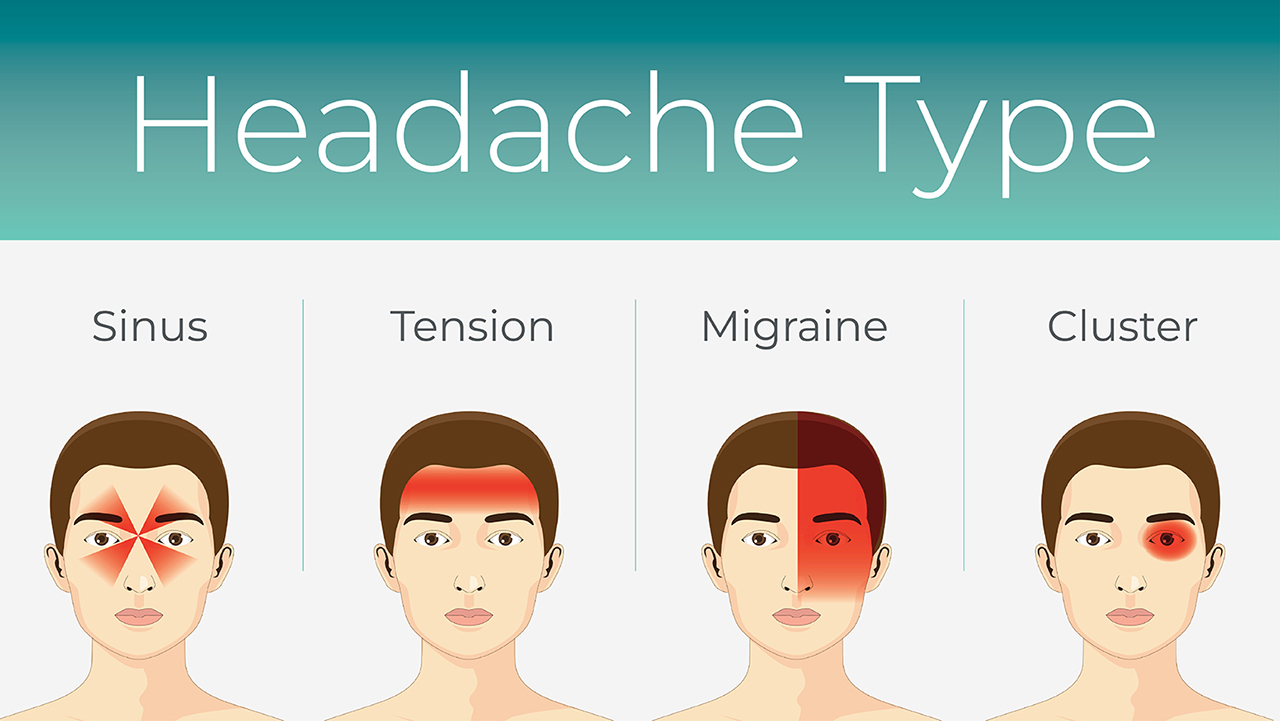
Migraine is a chronic and recurring form of headache characterized by intense throbbing or pressure, usually on one side of the head. Migraines can last from a few hours to three days and are often associated with other symptoms such as increased sensitivity to light, sound, as well as nausea and vomiting. Unlike regular headaches, migraine attacks can significantly affect people's daily functioning and quality of life.
What is a migraine aura?
Migraine aura is a specific complex of neurological symptoms that appear before or together with a migraine headache. An aura can last from a few minutes to an hour and affects about a third of people who experience migraines. Symptoms of an aura are varied and can include visual disturbances, speech or thinking problems, motor disturbances or even sensory changes. The aura phenomenon is related to the phenomenon of cortical heartbeat, which is the process of hyperactivity of neurons in the cerebral cortex and subsequent inhibition of their activity.
Causes of migraine
Migraine is a complex neurological disorder, the causes of which are still not fully understood, but scientific research reveals that migraine is caused by an interaction of various genetic, environmental and physiological factors. This interaction causes changes in brain chemistry, cerebrovascular reactions, and nervous system dysfunctions that together lead to migraine attacks.
Genetic factors
Research shows that genetics play a role in the development of migraines. Individuals with a family history of migraine sufferers are more likely to experience migraine attacks. Scientists have identified several genetic mutations that can increase the risk of migraines, but migraines involve more than just one gene, but many genetic factors that influence individuals' susceptibility to migraines in different ways.
Brain chemical imbalance
Imbalances in neurotransmitters, particularly serotonin and calcitonin gene-related peptide (CGRP), are also linked to migraines. Fluctuations in serotonin levels can affect cerebral blood vessel constriction and dilation, and CGRP is actively involved in regulating the inflammatory process associated with migraine attacks.
Changes in cerebral vascular activity
Migraines were previously thought to be associated only with cerebral vasodilation. Migraine is now known to be a much more complex disorder that also involves pain sensitivity mediated by nerve signals. However, cerebrovascular reactivity is still considered an important factor in the development of migraine.
Trigeminovascular system
Migraine attacks also involve the trigeminovascular system, which is the blood and nerve system in the brain and face area. When this system is activated, substances are released that cause inflammation of blood vessels and the transmission of pain signals to the brain, which are perceived as migraine pain.
The environmental factors
A variety of environmental factors can trigger migraine attacks in those who are prone to migraines. These include stress, consumption of certain foods and drinks (such as alcohol, caffeine), hormonal changes (such as the menstrual cycle in women), too much or too little sleep, exercise, changes in weather, and strong lights or sounds.
Hormonal changes
In women, migraines are often associated with hormonal changes, especially fluctuations in estrogen levels. This explains why women experience more frequent migraine attacks during menstruation, pregnancy or early menopause.
Although the causes of migraine are complex and individual, understanding these factors helps to better manage migraine attacks and reduce their frequency and severity. With appropriate treatment and avoidance of known triggers, many migraine sufferers can significantly improve their quality of life.
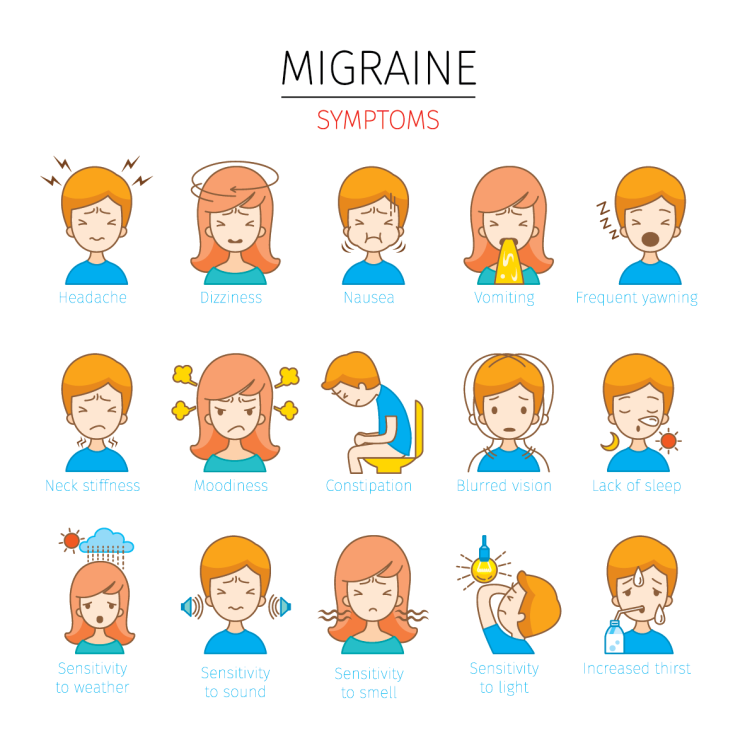
Symptoms
Migraine is a complex neurological disorder accompanied by various symptoms that differ in intensity, duration and impact on a person's quality of life. A migraine attack usually goes through several phases, each of which can have different symptoms. These symptoms not only include a severe, throbbing headache, but also several other sensations that may begin immediately before, during, or after the headache.
Prodromal phase (pre-primary symptoms)
Before a migraine attack, which can begin hours to days before the headache, individuals may experience so-called prodromal symptoms, including:
- Fatigue or lack of energy
- Constipation or, on the contrary, diarrhea
- Mood swings, including depression or sudden highs
- Cravings for desired foods
- Disturbed sleep
- Frequent yawning
Aura phase
Aura is present in about one-third of migraine sufferers. Aura symptoms are temporary neurological disturbances that usually last from 20 minutes to one hour. Aura can include:
- Visual disturbances such as flickering, seeing spots or lines, loss of field of vision.
- Numbness or weakness of the hands, face or speech, usually on one side of the body.
- Speech disorders, difficulty speaking or understanding words.
- In rare cases, motor disturbances may occur, including loss of coordination or even paralysis.
Headache phase
Headache is a migraine symptom that is commonly associated with this disorder. Pain can be:
- Intense, throbbing or pressure, usually localized on one side of the head.
- Strengthened by physical activity.
- Accompanied by increased sensitivity to light (photophobia), sounds (phonophobia) or smells.
- Nausea and vomiting are common symptoms.
- Duration 4 to 72 hours if untreated.
Post-attack phase
After a migraine attack, when the headache and other symptoms go away, individuals may feel exhausted or, conversely, re-energized. This phase may include:
- Fatigue and the need to rest.
- Muscle pain, especially in the neck area.
- Psychological symptoms such as depression, euphoria, or ruminations on past attacks.
- Difficulty concentrating or understanding.
The intensity and occurrence of migraine symptoms can vary between individuals, and the frequency of attacks can range from a few times a week to the rare occurrence of a migraine once a year. Although there is currently no cure for migraine, effective treatments can help manage symptoms and reduce the frequency and severity of attacks. Treatment strategies include pain medications and preventative treatments, lifestyle changes, stress management techniques, and alternative therapies such as acupuncture or biofeedback.
What is the effect of migraine on work, family and social life?
Migraine is not only a chronic, recurring form of headache, but also a condition that has a significant impact on personal, professional and social life. Migraine attacks, characterized by intense, throbbing pain on one side of the head, can last from several hours to three days and are often accompanied by nausea, vomiting, and sensitivity to light and sound. The impact of this complex of symptoms on a person is great and often goes beyond physical suffering.
In the field of work, migraines can significantly reduce productivity and efficiency. The difficulty concentrating, memory problems, and fatigue that often accompany migraines can interfere with daily tasks, reduce work productivity, and even require time off work. In the long run, this can have negative consequences for a professional career, including missed work days, slowed career growth and financial losses.
The impact of migraines on family life is also significant. During attacks, a person often becomes emotionally vulnerable, and the pain makes it difficult to form and maintain relationships with family members. This can cause strain in the relationship, as the person may feel misunderstood or burdened with guilt about their inability to actively participate in family activities. Raising children and family responsibilities can become an extremely heavy burden, especially during intense migraine periods.
Migraines also present challenges in social life. Social gatherings, events and interacting with friends can become difficult due to the fear of a migraine. This can promote avoidance behavior where a person refuses to participate in social activities in order to avoid pain triggers. Gradually, this can lead to social isolation, depression and increased levels of anxiety, reducing the overall quality of life.
It is important to note that the impact of migraines varies from person to person and depends on many factors, including the frequency and intensity of the attacks, and personal and professional circumstances. Therefore, migraine management, including medication, lifestyle modification, and stress management practices, is essential to reduce the impact of migraine on personal, professional, and social life.
Information sources
- "Headache: The Journal of Head and Face Pain"
- The Journal of Headache and Pain
- Migraine Research Foundation
- World Health Organization
# migrena






