Hepatitis C is a viral infection that damages the liver and can cause both mild and severe forms of the disease, including chronic liver inflammation, cirrhosis, and hepatocellular carcinoma (liver cancer). This infection is caused by the Hepatitis C virus (HCV), which is transmitted through contaminated blood and other body fluids. Hepatitis C is a global public health issue, often remaining unnoticed for a long time due to its asymptomatic initial stage.
The Hepatitis C virus can cause both acute and chronic infections. Acute infections are usually asymptomatic or have mild symptoms, such as fatigue, abdominal pain, and sometimes jaundice. However, about 75-85% of those infected experience a chronic infection, which can progress to serious liver diseases. Chronic hepatitis C is especially dangerous as it can be asymptomatic for years or even decades until serious liver damage occurs.
What symptoms does hepatitis C cause?
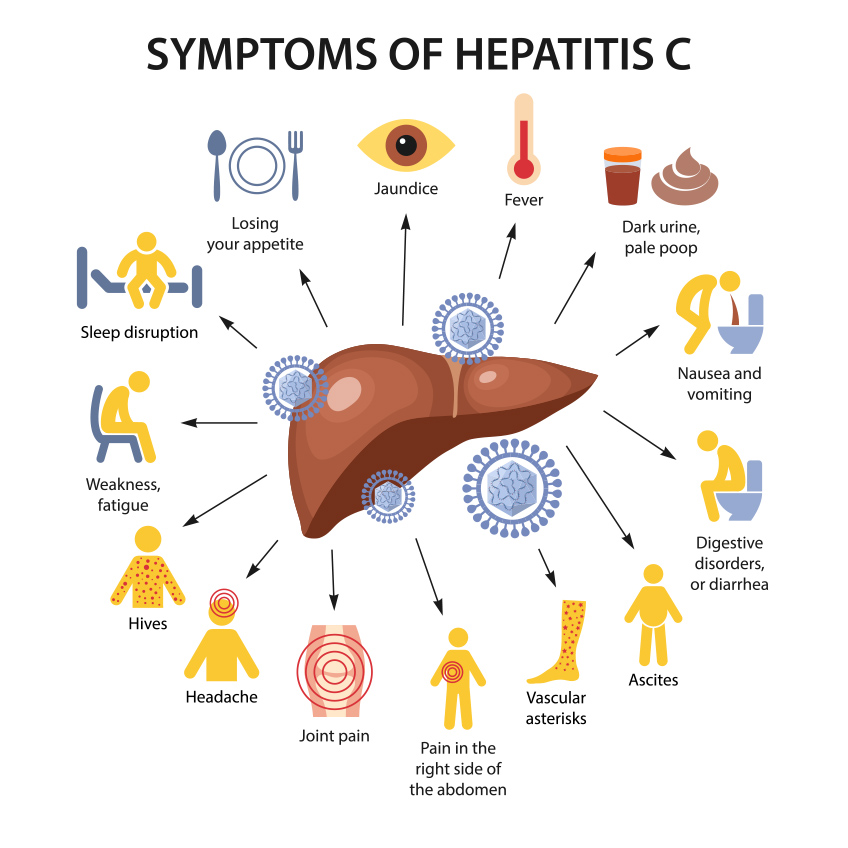
The symptoms of Hepatitis C vary and can range from mild to very severe, and sometimes the disease can be completely asymptomatic, especially in the early stages. Hepatitis C causes inflammation of the liver, and its symptoms often only appear in the advanced stages of the disease, complicating early diagnosis.
During the acute phase of Hepatitis C, which usually lasts the first 6 months after infection, symptoms can be mild or nonexistent. Some patients may experience general fatigue, weakness, abdominal pain, loss of appetite, nausea, vomiting, or fever. Jaundice may also occur – a yellowing of the skin and whites of the eyes due to increased bilirubin in the blood, which is a direct sign of liver function impairment. Another symptom can be dark urine and light-colored stools.
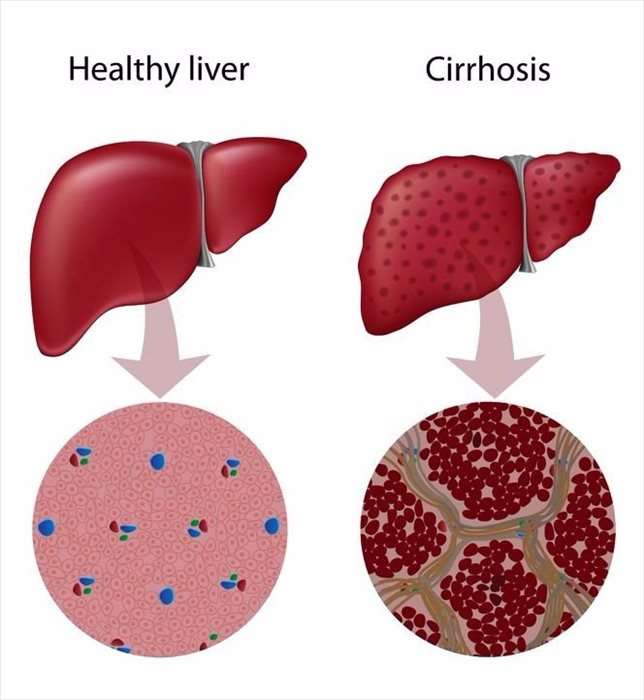
The chronic phase of Hepatitis C is characterized by similar but often more severe symptoms. Over time, if hepatitis C is not treated, more serious liver damage can develop, including liver cirrhosis – a condition where normal liver tissue is replaced with scar tissue, hindering normal liver function. Symptoms of cirrhosis include abdominal bloating due to fluid accumulation (ascites), bleeding from the digestive tract, a significantly enlarged liver, hepatic encephalopathy (mental disturbances due to liver failure), and spider angiomas on the skin.
In the most severe case, chronic hepatitis C infection can lead to hepatocellular carcinoma, which is the primary type of liver cancer. In this case, symptoms may include pain in the right side of the abdomen, abnormal weight loss, and dilated blood vessels on the abdominal skin.
It should be emphasized that the symptoms of hepatitis C are highly individual and depend on many factors, including the patient's age, sex, overall health condition, other coexisting diseases, and the characteristics of the virus. For this reason, hepatitis C diagnosis is often made after appropriate blood tests, rather than solely based on symptoms. Early diagnosis and treatment are crucial to prevent the progression of the disease and its complications.
How does hepatitis C spread?
Hepatitis C is highly infectious and can remain infectious in the external environment for a long time. The main method of transmission is direct blood contact with an infected person.
One of the most common ways of infection is through unsafe injection practices. This includes the use of dirty or shared needles during drug use. There is also a higher risk among individuals who use intravenous drugs or have had unsafe ear piercing or tattoo procedures if these procedures used infected tools.
In previous decades, hepatitis C was often transmitted through blood products and organ transplants, as there were no effective testing methods for blood donors at that time. In modern medicine, thanks to strict blood product testing procedures, this transmission route has become very rare.
Sexual transmission is a less common way of spreading hepatitis C. Although the risk is significantly lower than through blood contact, it still exists, especially among individuals with multiple sexual partners or those with other sexually transmitted infections, such as HIV.
Transmission from mother to child (vertical transmission) during childbirth is also possible but not common. Although this risk is not high, it increases if the mother has chronic hepatitis C or HIV.
An important note is that hepatitis C does not spread through everyday social contact, such as hugging, handshakes, or using common household items, such as dishes or toilets. It is also not transmitted through food or water.
Control and prevention measures include safe and responsible behavior, especially related to blood contact. This means avoiding shared needle use, ensuring that all medical, tattooing, and ear piercing procedures are performed using sterile materials, and undergoing regular health checks, especially if a person belongs to a higher risk group.
Hepatitis C can cause certain complications
Hepatitis C, a chronic viral liver infection, can lead to several serious complications, especially if it is not properly treated. These complications can include long-term liver damage and other related health problems.
- Liver cirrhosis. One of the most common and serious complications of hepatitis C is liver cirrhosis. This condition involves the gradual replacement of normal liver tissue with scar tissue (fibrosis), disrupting liver function. Cirrhosis can develop over several decades and cause liver failure, ascites (fluid accumulation in the abdomen), bleeding from stomach and esophageal varices, and hepatic encephalopathy, characterized by brain function disorders.
- Hepatocellular carcinoma (liver cancer). Individuals with chronic hepatitis C are at an increased risk of developing hepatocellular carcinoma, the primary type of liver cancer. This risk is particularly high in patients with cirrhosis. Hepatocellular carcinoma may present as abdominal pain, weight loss, and severe fatigue, although it is often asymptomatic in the early stages.
- Liver failure. Advanced liver cirrhosis can progress to liver failure, a life-threatening condition. This condition is characterized by the liver's inability to perform vital functions, such as toxin removal from the blood, protein synthesis, and blood clotting regulation.
- Portal hypertension. Cirrhosis can lead to portal hypertension, which is increased blood pressure in the liver's portal vein. This can cause bleeding from the digestive tract, especially from varicose veins in the esophagus and stomach.
- Immune system disorders. Hepatitis C can cause various immune system disorders, including cryoglobulinemia – a condition characterized by the accumulation of certain proteins, called cryoglobulins, in the blood, which can cause inflammation and damage in various parts of the body.
- Mental health problems. Hepatitis C infection can also affect mental health, including depression and anxiety disorders, which may be related to both hepatitis C and its treatment effects.
These complications highlight why it is important to diagnose and effectively treat hepatitis C early. Early treatment can significantly reduce the risk of developing severe complications and improve the quality of life for affected individuals.
Can hepatitis C be prevented, and how to protect yourself?
Preventing hepatitis C is a crucial public health area, aiming to reduce the number of new infections and prevent the spread of the disease. Hepatitis C is transmitted through contaminated blood, so the primary goal of prevention is to reduce the risk of encountering infected blood. These prevention strategies include both public health initiatives and individual behavioral changes.
- Safe blood transfusions and organ transplants: Ensuring that all blood products and transplanted organs are thoroughly tested for hepatitis C. This practice is particularly important in medical facilities and is already widely implemented in many countries.
- Sterile medical tools: Ensuring that all medical tools, especially those used for blood procedures, are properly sterilized. This includes not only surgical instruments but also needles, syringes, and other tools used in medical and dental practices.
- Safe drug use: Providing education about the risks associated with unsafe intravenous drug use.
- Safe practices for tattoos and ear piercing: Ensuring that all tattooing and ear piercing procedures are performed using sterilized tools. This also includes educating about the risks and adhering to proper practices.
- Information and education: It is important to provide information about the ways hepatitis C is transmitted and prevention strategies. This includes information campaigns, education in schools, workplaces, and health care facilities.
- Sexual education and safety: Although sexual transmission is not the primary way hepatitis C spreads, it is important to inform people about the risk, especially those with multiple sexual partners or other sexually transmitted infections.
- Early detection: Regular hepatitis C testing for those who belong to higher-risk groups, such as individuals using intravenous drugs, people with multiple sexual partners, or those who received a blood transfusion or organ transplant before the introduction of blood testing procedures.
These prevention measures are vital to reduce the spread of hepatitis C and prevent new infections. It is also important to emphasize that public health policy and individual responsibility are key factors in preventing this infection.
Information sources:
- World Health Organization (WHO)
- Centers for Disease Control and Prevention (CDC)
# hepatitas c