
Liver cirrhosis is a chronic liver disease caused by long-term damage to liver tissue. Liver cirrhosis develops for various reasons, including prolonged alcohol consumption, viral hepatitis B and C infections, autoimmune liver damage, genetic disorders such as hemochromatosis and Wilson's disease, and toxic damage (e.g., caused by medications). The essence of liver cirrhosis is a gradually progressing fibrosis process, in which normal liver tissue is replaced by connective tissue (fibrosis) scars. This disrupts the normal structure and functions of the liver as the liver cells (hepatocytes) die and are replaced by ineffective scar tissue.
The development of liver cirrhosis is characterized by two stages: compensated and decompensated. In the compensated stage, the liver is still able to perform most of its functions, and symptoms can be mild or completely unnoticeable. Gradually, as the disease progresses, the liver can no longer function properly, leading to decompensated cirrhosis, where serious symptoms and complications occur. These symptoms can include yellowing of the skin and eyes (jaundice), abdominal bloating due to fluid accumulation (ascites), bleeding from the gastrointestinal tract, mental disorders (hepatic encephalopathy), and blood clotting disorders.
The treatment of liver cirrhosis depends on its main cause: cessation of alcohol consumption, antiviral drugs for treating hepatitis, medications to control autoimmune liver diseases, etc. It is important to emphasize that liver cirrhosis is an irreversible condition, so treatment is usually aimed at slowing the progression of the disease and managing complications. In advanced cases, a liver transplant may be necessary. In addition, the patient's lifestyle plays an important role, including a balanced diet, regular health checks, and overall health care.
How does liver cirrhosis develop?
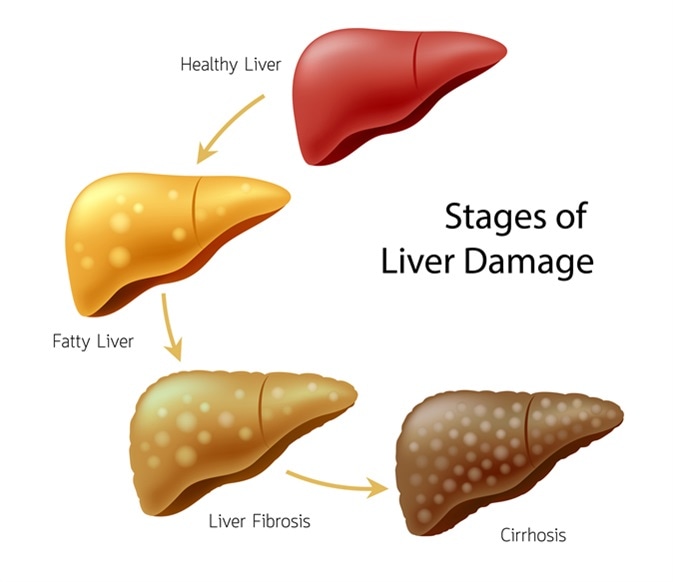
The development of liver cirrhosis is a complex and gradually progressing process that can take several decades. This condition is characterized by progressive fibrosis of the liver tissue (formation of scar tissue) and changes in the normal structure of the liver, which ultimately disrupt liver functions. The development of liver cirrhosis goes through several stages:
Initial damage
Firstly, the development of liver cirrhosis is caused by long-term damage to liver tissue, which can be caused by various reasons, such as excessive alcohol consumption, viral hepatitis, autoimmune diseases, genetic disorders, or constant exposure to toxic substances. These factors cause inflammation and cell death in the liver.
Inflammation and fibrosis
Long-term inflammation in the liver promotes the activation of fibroblasts (scar tissue-forming cells). Fibroblasts produce collagen and other connective tissue components, which replace damaged liver cells. This process is called fibrosis. In the initial stages, fibrosis can be reversible, but over time, with continuous damage, it becomes irreversible.
Regeneration and scar tissue formation
The liver tries to recover after damage, but due to continuous inflammation and fibrosis, the regeneration is not complete or orderly. Instead of normal liver tissue, disorganized regenerative tissue forms, consisting of small liver nodules surrounded by scar tissue.
Changes in liver structure and function
Due to scar tissue and disorganized regeneration, the liver structure changes, disrupting the normal blood flow through the liver and nutrient metabolism. This impairs the liver's ability to perform its functions, such as toxin removal, protein synthesis, and drug metabolism.
Complications
As liver cirrhosis progresses, complications arise, such as portal hypertension (increased blood pressure in the liver's portal vein), ascites (fluid accumulation in the abdominal cavity), varicose veins (especially in the esophagus, which can cause bleeding), hepatic encephalopathy (brain function disorder due to toxin accumulation in the blood), and other serious conditions.
The rate of progression and impact of liver cirrhosis can vary depending on the cause of the damage, individual patient health factors, and lifestyle choices. Early diagnosis and proper treatment, as well as controlling the main causes (e.g., cessation of alcohol consumption, antiviral treatment for hepatitis), can slow down the progression of the disease and reduce the risk of complications.
Causes of the disease
Liver cirrhosis is a chronic liver disease characterized by fibrosis of the liver tissue (formation of scar tissue) and changes in the normal structure of the liver, leading to impaired liver function. This disease can be caused by various factors, whose effects can last a long time. The most important causes of liver cirrhosis are:
- Alcoholic liver disease: Prolonged and excessive alcohol consumption is one of the most common causes of liver cirrhosis. Alcohol can directly damage liver cells, promoting an inflammatory process and the development of fibrosis.
- Viral hepatitis: Especially hepatitis B and C. These viruses cause inflammation in the liver, and long-term inflammation can lead to the formation of scar tissue and eventually liver cirrhosis.
- Fatty liver disease: Associated with fat accumulation in the liver, often linked to obesity, diabetes, hyperlipidemia, and metabolic syndrome. Fatty liver disease can progress to fatty hepatitis and later to cirrhosis.
- Autoimmune liver diseases: Such as autoimmune hepatitis, where the immune system improperly attacks liver cells, causing inflammation and fibrosis.
- Genetic disorders: Such as hemochromatosis (excessive iron accumulation in the body, damaging the liver) and Wilson's disease (a rare genetic disorder that causes copper accumulation in the body, including the liver).
- Exposure to toxic substances: The effects of certain toxins, such as medications, or chemicals, such as methanol or certain industrial toxins, can cause liver damage.
- Primary biliary cirrhosis and primary sclerosing cholangitis: These are conditions that damage the liver's bile ducts, causing inflammation and eventually fibrosis.
Risk factors that increase the likelihood of developing liver cirrhosis include:
- Excessive alcohol consumption: This is one of the main risk factors, especially when a large dose of alcohol is consumed over a long period.
- Infections: Hepatitis B and C viruses are major liver cirrhosis risk factors worldwide.
- Obesity: Especially important in the case of fatty liver disease and its progression to liver cirrhosis.
- Genetic factors: Heredity can play a role in some types of cirrhosis, such as hemochromatosis.
- Immune system disorders: Autoimmune liver diseases are a risk factor.
- Use of certain medications: Long-term use of certain medications that can be toxic to the liver.
Timely diagnosis and proper management of the main causes of liver cirrhosis can prevent or slow down liver damage progression. It is also important to control general health aspects, such as maintaining a normal weight, healthy diet, and regular physical activity.
Symptoms
Liver cirrhosis is a chronic liver disease that gradually damages the liver tissue, causing its fibrosis and changes in the normal structure of the liver. This condition can be asymptomatic for a long time, but as the disease progresses, various symptoms and signs appear:
- Fatigue and weakness: These are common early symptoms caused by a general decrease in body efficiency and the accumulation of toxins, as the liver cannot properly remove harmful substances from the blood.
- Yellowing of the skin and eyes (jaundice): Due to the accumulation of bilirubin, a natural pigment usually removed by the liver, in the blood. This gives the skin and the whites of the eyes a yellowish tint.
- Abdominal bloating and fluid accumulation (ascites): Caused by a decrease in the production of albumin, a major blood protein, in the liver and increased blood pressure in the liver veins.
- Weight loss and loss of appetite: Due to digestive problems and a general deterioration of the body's condition.
- Bleeding and bruising: Liver insufficiency disrupts blood clotting, so patients may bleed more easily or develop bruises.
- Mental disorders (hepatic encephalopathy): The accumulation of toxins, especially ammonia, in the blood can affect brain function, causing confusion, lack of concentration, behavioral changes, and in severe cases - loss of consciousness.
- Itching of the skin: Due to the accumulation of toxins in the blood, which irritate the skin.
- Subcutaneous blood vessel "stars" (telangiectasia): Small, star-shaped blood vessels that appear on the skin.
- Heavy bleeding from minor injuries: Due to disrupted blood clotting.
- Severe pain on the left side of the body: May occur due to an increase in liver size or ascites.
- Change in urine color: Darker urine due to the excretion of bilirubin.
- Change in stool color: May become lighter due to reduced bilirubin excretion into the intestines.
It is important to emphasize that these symptoms may not be specific to liver cirrhosis and may indicate other health problems. Therefore, if any of these symptoms occur, it is necessary to consult a doctor. Early diagnosis and proper treatment can stop or slow down the progression of the disease, reduce the risk of complications, and improve quality of life.

What complications does liver cirrhosis cause?
As liver cirrhosis progresses, it can cause various serious and life-threatening complications:
Portal hypertension
One of the main complications of liver cirrhosis, manifested by increased blood pressure in the liver veins. Liver fibrosis obstructs normal blood flow through the liver, causing pressure in the portal vein. This can lead to the expansion of blood vessels (varicose veins) and bleeding, especially in the esophagus and stomach.
Ascites
Fluid accumulation in the abdominal cavity caused by portal hypertension and a decrease in protein (albumin) production in the liver. Ascites can cause abdominal bloating, discomfort, and breathing difficulties.
Hepatic encephalopathy
A brain function disorder caused by the accumulation of toxins, especially ammonia, in the blood due to the liver's reduced ability to remove them. Symptoms may include confusion, behavioral changes, motor disorders, and in severe cases – loss of consciousness.
Jaundice
Due to liver insufficiency, inability to remove bilirubin, it accumulates in the blood, giving the skin and the whites of the eyes a yellowish tint.
Risk of infections
Liver cirrhosis reduces the body's resistance to infections, especially abdominal cavity infections, such as spontaneous bacterial peritonitis, which is a complication of ascites.
Bleeding and clotting disorders
Liver insufficiency disrupts the synthesis of blood clotting factors, increasing the risk of bleeding, especially in the gastrointestinal tract.
Rupture of varicose veins
Increased pressure in blood vessels, especially in the esophagus and stomach area, can lead to their expansion (varicose veins) and rupture, causing dangerous internal bleeding.
Hepatocellular carcinoma (liver cancer)
Liver cirrhosis is one of the main risk factors for liver cancer. Continuous inflammation and regeneration of liver tissue can lead to abnormal cell growth and cancer development.
Kidney function disorders
Severe liver cirrhosis can negatively affect kidney function, due to changes in circulation and hormonal regulation disorders, causing hepatorenal syndrome.
Weight loss and muscle mass decrease
Due to decreased appetite, malabsorption, and metabolic disorders.
The prevention and treatment of these complications are important aspects of managing liver cirrhosis. This includes regular medical check-ups, lifestyle changes (e.g., abstaining from alcohol, healthy diet), medications for reducing blood pressure in the liver, managing ascites, and preventing and treating infections. In advanced cases, a liver transplant may be necessary.

Lifestyle changes
Prevention methods include various lifestyle changes, medical measures, and regular health check-ups to prevent the development of liver cirrhosis or slow its progression.
Healthy lifestyle
This is a key factor in the prevention of liver cirrhosis. It is important to:
- Reduce alcohol consumption or completely abstain from it
- Maintain a healthy weight
- Eat healthy food
- Avoid harmful substances
Infection control
- Hepatitis vaccination
- Regular health check-up
Management of chronic liver diseases
- Regular doctor visits
- Proper treatment
Avoidance of toxins and chemicals
- Protect yourself from harmful chemicals
- Regular health check-up
It is important to emphasize that the prevention of liver cirrhosis is a long-term process that requires consistent attention to health and regular medical check-ups. Early intervention and lifestyle changes can significantly reduce the risk of liver cirrhosis and its associated complications.
Information sources
- Harrison's Principles of Internal Medicine
- Cecil Essentials of Medicine
- Mayo Clinic Proceedings
- New England Journal of Medicine
- American Journal of Gastroenterology
# kepenu ciroze






