Tuberculosis, commonly known as TB, is an infectious disease caused by the Mycobacterium tuberculosis (Mtb) bacterium. This bacterium most often infects the lungs, causing pulmonary tuberculosis, but it can also affect other organs in the body such as the bones, urinary tract, nervous system, lymphatic system, and others, leading to what is known as extrapulmonary tuberculosis.
Tuberculosis spreads through the air when a person with active pulmonary tuberculosis releases bacteria into the air by coughing, sneezing, speaking, or singing. These bacteria can remain suspended in the air for a long time and infect others who inhale the contaminated air.
It is important to note that not everyone who becomes infected with the TB bacterium develops active tuberculosis. Most infected individuals (about 90%) develop latent tuberculosis, where the bacteria remain inactive and cause no symptoms. These individuals are not contagious. However, latent tuberculosis can become active, especially when a person’s immune system becomes weakened—for example, due to HIV infection, old age, or immunosuppressive treatment.
Tuberculosis (TB) spreads through the air when a person with active pulmonary tuberculosis releases bacteria by coughing, sneezing, speaking, or singing. TB bacteria (Mycobacterium tuberculosis) can remain in the air for several hours and may be inhaled by others, leading to infection.
When a person inhales TB bacteria, the bacteria travel through the respiratory tract and settle in the lungs, where they can begin to multiply. While the immune system often prevents active infection by forming a protective capsule around the bacteria (resulting in latent tuberculosis), in some cases the bacteria remain viable and later become active when immunity weakens.
Although tuberculosis is infectious, it does not spread easily. Infection usually requires prolonged and close contact with an infected person. This is why TB most commonly spreads among family members, close contacts, and coworkers. Early detection and treatment of TB cases is essential to prevent its spread.
TB transmission is also associated with social and economic factors. For example, tuberculosis is more common among people living in poverty, those with weakened immune systems, or individuals with limited access to healthcare. TB is also more prevalent among immigrants from high-burden countries and people living in crowded institutions such as prisons or refugee camps.
Tuberculosis (TB) can cause different symptoms depending on the part of the body that is infected. However, most individuals infected with Mycobacterium tuberculosis initially develop latent tuberculosis, which causes no symptoms and is not contagious.
Pulmonary Tuberculosis
When infection affects the lungs (pulmonary tuberculosis), the most common symptoms are:
A cough lasting three weeks or longer
Coughing up blood or mucus
Chest pain, especially when breathing or coughing
Weakness or fatigue
Unexplained weight loss
Night sweats
Fever
Extrapulmonary Tuberculosis
When TB affects other parts of the body (extrapulmonary tuberculosis), symptoms vary depending on the organ involved. For example:
Bone tuberculosis may cause pain in the affected bone and potential fractures
Kidney tuberculosis may cause blood in the urine or urinary tract infections
Tuberculosis of the nervous system (brain or spine) may cause headaches, loss of consciousness, or paralysis
Regardless of type, TB may also cause general symptoms such as fever, night sweats, weakness, fatigue, and unexplained weight loss.
Tuberculosis can be very serious, especially if untreated. However, when properly diagnosed and treated in time, most cases are curable. Anyone experiencing the symptoms listed above should seek medical attention.
Healthcare professionals use several methods to diagnose tuberculosis (TB). The primary test, known as the TB skin test or Mantoux test, is used to determine whether a person is infected with Mycobacterium tuberculosis. A small amount of TB protein (tuberculin) is injected under the skin, and the area is checked for redness or swelling after 48–72 hours.
TB infection can also be detected using blood tests such as QuantiFERON®-TB Gold Plus (QFT-Plus) and T-SPOT®.TB. These tests measure the immune system’s response to TB bacteria.
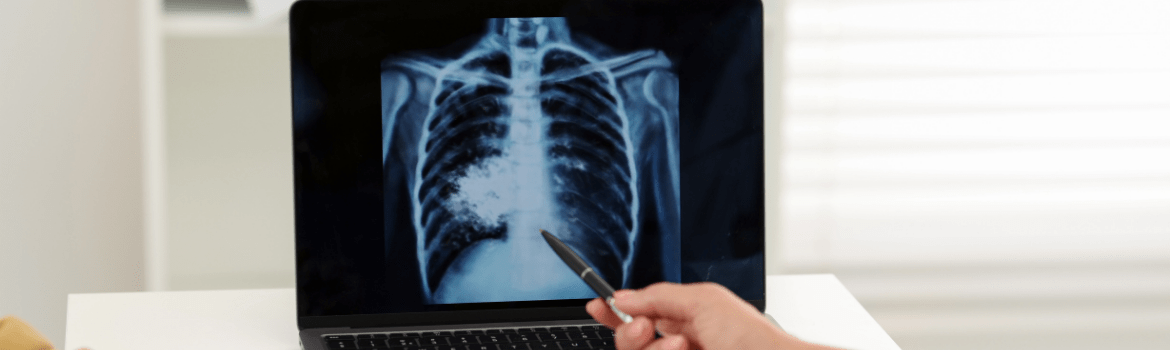
If a skin or blood test is positive, additional tests are needed to confirm whether the person has active TB disease. These may include a chest X-ray and/or microscopic examination of sputum samples.
Treatment depends on the type of infection.
Latent tuberculosis (bacteria present but inactive) is usually treated with one or two medications to prevent progression to active TB.
Active tuberculosis requires long-term antibiotic therapy. Treatment typically lasts at least six months and involves a combination of four drugs—isoniazid, rifampicin, pyrazinamide, and ethambutol—for the first two months, followed by isoniazid and rifampicin for an additional four months.
Strict adherence to treatment is essential. Stopping treatment early can lead to drug resistance and recurrence of the disease.
Drug-resistant TB is a growing global health concern. Resistance develops when TB bacteria mutate and become unresponsive to certain antibiotics. This may occur when treatment is incomplete or when ineffective medications are used.
Two main types of resistance exist:
Multidrug-resistant tuberculosis (MDR-TB) – resistant to at least isoniazid and rifampicin
Extensively drug-resistant tuberculosis (XDR-TB) – resistant to isoniazid, rifampicin, at least one fluoroquinolone, and one second-line injectable drug
Drug-resistant TB is harder to treat, requires longer and more complex treatment, and has more side effects.
The World Health Organization (WHO) and other global health institutions are working to combat drug-resistant TB through improved diagnostics, new medications, and stronger disease-control strategies.
Individual consequences
If not properly treated, TB can cause severe and long-lasting health problems:
Lung damage such as fibrosis, respiratory failure, or bleeding
Damage to other organs, including kidneys, bones, and the nervous system
Psychological burden, including stress, anxiety, and depression
Public health consequences
Tuberculosis is one of the leading infectious causes of death worldwide. Drug-resistant forms pose major challenges to healthcare systems.
TB also causes economic hardship by reducing productivity and increasing healthcare costs. Social stigma may also affect affected individuals.
Effective prevention and control strategies are essential for reducing TB incidence, mortality, and drug resistance.
Vaccination
The BCG vaccine (Bacillus Calmette-Guérin) is widely used to protect infants and children in high-risk areas from severe forms of TB.
Medical prophylaxis
Individuals at high risk—such as recent contacts of TB cases or those with weakened immunity—may receive preventive antibiotic therapy to stop latent TB from becoming active.
Early detection and treatment
Identifying and treating TB cases early is the most efficient way to prevent transmission. Expanding diagnostic services is crucial.
Infection control
In healthcare settings and crowded environments, infection-control measures—good ventilation, appropriate respirators, and isolation of infectious patients—are essential.
Tuberculosis is a complex infectious disease that significantly impacts individuals and societies worldwide. Although it primarily affects the lungs, it can spread to other organs, causing severe long-term consequences. TB also has psychological impacts and poses serious challenges to public health systems.
World Health Organization. (2022). Tuberculosis.
Centers for Disease Control and Prevention. (2022). TB Disease: General Information.
Mayo Clinic. (2021). Tuberculosis.
American Lung Association. (2022). Diagnosing Tuberculosis (TB).
World Health Organization. (2023). Multidrug-resistant tuberculosis (MDR-TB).
Centers for Disease Control and Prevention. (2021). TB Prevention.