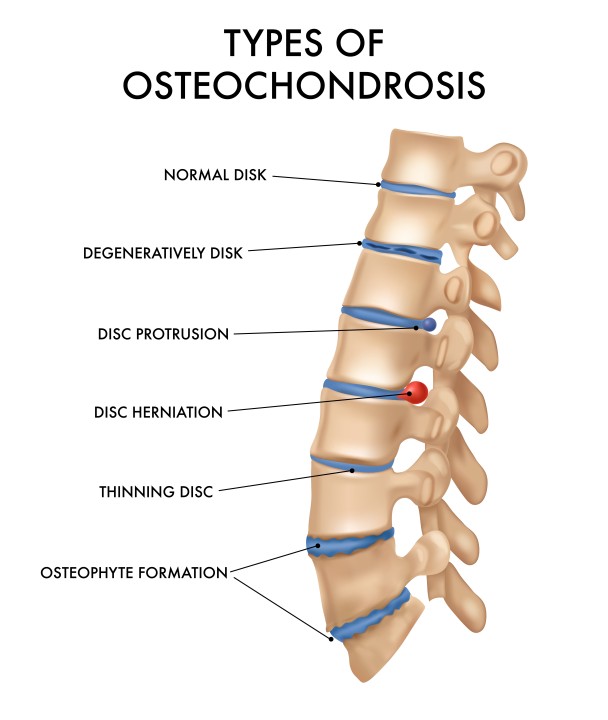
Osteochondrosis is a degenerative disease affecting bones and joints, most commonly manifesting in the spine, though it can also affect other parts of the body. It is a complex pathology associated with changes in the structural and functional condition of the intervertebral discs, which act as cushions between the vertebrae. The progression of osteochondrosis is slow and progressive, and its primary factors include age, genetic predisposition, excessive physical strain, improper posture, obesity, and other related health disorders.
As osteochondrosis progresses, the intervertebral discs begin to dry out and lose their elasticity, making them less resistant to various loads. This can lead to disc inflammation or even herniation, causing nerve compression and pain. Additionally, degenerative changes in the vertebrae can lead to the formation of osteophytes (bone growths), which can also irritate or compress nerves and other tissues.
What causes osteochondrosis?
Osteochondrosis is a complex degenerative disease affecting the joints and intervertebral discs, especially in the spine. While the exact causes of this disease can vary, the onset of osteochondrosis is conditioned by various biomechanical, genetic, and environmental factors. The main causes of osteochondrosis are:
- Age: This is one of the primary causes of osteochondrosis onset. The aging process naturally reduces the elasticity and resilience of the intervertebral discs, as they lose moisture and proteins needed to maintain their structure and function.
- Genetics: Genetics play an important role in the development of osteochondrosis. Studies indicate that the disease can be hereditary, and certain genes may increase susceptibility to the disease.
- Physical strain and occupational activities: Prolonged or improper physical strain, especially associated with repeated lifting, bending, or long periods of sitting, can increase the risk of developing osteochondrosis. People engaged in heavy physical work or occupations requiring long periods of sitting or monotonous movements are more vulnerable.
- Improper posture: Prolonged improper posture, especially while sitting at a computer or using a mobile phone, can cause disproportionate strain on the spine, increasing the risk of wear on the intervertebral discs.
- Trauma: Spinal traumas, such as impacts or injuries sustained while playing sports, can cause or worsen the condition of osteochondrosis.
- Obesity and poor diet: Being overweight increases pressure on spinal discs and joints, and poor nutrition can interfere with the supply of necessary nutrients essential for bone and joint health.
- Sedentary lifestyle: Lack of physical activity weakens spinal muscles and reduces flexibility, which can contribute to the development of osteochondrosis.
- Hormonal changes: Certain hormonal changes, such as menopause in women, can affect bone density and the health of intervertebral discs.
These factors can interact and reinforce each other, so osteochondrosis prevention and treatment include various aspects, including lifestyle changes, physical activity, and professional medical intervention. By paying attention to these factors, it is possible to reduce the risk of osteochondrosis onset or slow its progression.

Symptoms of the disease
Osteochondrosis, a degenerative disease of the joints and bones, most commonly manifests in the spine, though it can also affect other joints. The symptoms of this disease can range from mild to very severe and depend on the stage of the disease, the affected area, and the individual characteristics of the patient. Here are some of the main symptoms of osteochondrosis:
Pain is the most common symptom of osteochondrosis. The pain can be localized in the affected area, such as the back or neck, and can spread to other parts of the body, such as the hands or legs. The nature of the pain can vary – from a stabbing or burning sensation to constant pain.
Patients often complain of difficulties in performing daily activities due to a reduced range of motion and stiffness in the affected area.
Numbness and tingling often occur in the hands, legs, or fingers, especially if osteochondrosis is associated with nerve compression.
Muscle weakness can occur in the affected body parts due to nerve compression, which can cause difficulties in performing simple activities or even a loss of the ability to hold objects.
Back pain is also a commonly occurring symptom associated with spinal osteochondrosis, especially in the lower back (lumbar region).
Cervical osteochondrosis can cause neck pain, which can spread to the head, causing headaches or even migraines.
Due to pain and discomfort, patients may unconsciously change their gait or posture to reduce pain.
Some patients experience a decrease in skin sensitivity or changes in the affected area.
Due to pain, stiffness, and other symptoms, patients may encounter difficulties in performing simple tasks, such as bending, reaching for objects, or even walking.
It should be noted that the symptoms of osteochondrosis can be similar to those of other skeletal and muscular system diseases, so it is important to consult a healthcare professional for accurate diagnosis and appropriate treatment. Early recognition of symptoms and proper treatment can help prevent the progression of the disease and improve the quality of life.
Treatment
The treatment of osteochondrosis is complex and often requires an integrated approach, involving various medical and healthcare disciplines. The primary goal of treatment is to reduce pain, improve function, and prevent the progression of the disease. The treatment plan depends on the stage of osteochondrosis, the affected area, and the individual needs of the patient. Here are some of the key aspects of osteochondrosis treatment:
Medication therapy
This includes pain-relieving medications (analgesics), anti-inflammatory drugs (non-steroidal anti-inflammatory drugs, NSAIDs), and muscle relaxants. Some patients may be prescribed antidepressants or anticonvulsants to control chronic pain.
Physiotherapy
Physiotherapy procedures, including therapeutic exercises, electrotherapy, ultrasound, or heat/cold therapy, can help reduce pain, improve the range of motion, and strengthen muscles.
Exercise therapy
Properly selected exercises are crucial in the treatment of osteochondrosis, as they help strengthen the back and abdominal muscles, improve posture, and reduce pressure on the intervertebral discs.
Chiropractic and manual therapy
For some patients, these procedures can help restore range of motion, reduce pain, and improve overall function.
Acupuncture
Some patients experience a reduction in pain and tension following acupuncture procedures.
Massage
Massage can help relax tense muscles, improve circulation, and reduce pain.
Psychological support
Psychological interventions, such as cognitive-behavioral therapy, can be beneficial in combating stress and depression caused by chronic pain.
Lifestyle changes
This includes weight control, quitting smoking, healthy eating, and creating an ergonomic workspace.
Interventional procedures
In some cases, injections, such as epidural steroid injections, may be applied to reduce pain and inflammation.
Surgical treatment
This is usually the last resort for severe forms of osteochondrosis, especially when other treatment methods are ineffective and there are serious nerve compression or stability issues.
It is important to note that the treatment of osteochondrosis is a long-term process, requiring patient commitment and regularly performed exercises and treatment procedures. It is also very important to closely collaborate with a doctor to create an individual and effective treatment plan.
The benefits of massage in treating osteochondrosis
One of the main benefits of massage is its ability to reduce pain. Massaging stimulates sensory receptors in the skin and tissues, which can help reduce the sensation of pain. Additionally, massage promotes the production of endorphins, natural pain-relieving substances in the body.
Osteochondrosis often causes muscle tension and stiffness, especially in the back and neck areas. Massage can help relax tense muscles, improving their elasticity and reducing discomfort.
During massage, blood circulation is improved, which helps promote the healing and regeneration of damaged tissues. Better blood flow also means more efficient delivery of oxygen and nutrients to the affected areas.
Massage can help improve flexibility and increase the range of motion, especially in the spinal area. This is important as osteochondrosis often causes limited mobility.
Massage is an excellent stress-reduction tool. Stress and tension can exacerbate osteochondrosis symptoms, so relaxation during a massage can have a positive impact on the overall condition of the patient.
Patients with osteochondrosis often experience sleep disturbances due to pain and discomfort. Massage can help improve sleep quality, reducing pain and relaxing the body.
There is evidence that regular massage can help strengthen the immune system, which is important for the body's resistance to diseases and infections.
Massage also positively affects emotional health. It can help reduce symptoms of anxiety and depression, which can accompany chronic pain syndromes like osteochondrosis.
It is important to emphasize that massage should be performed by a qualified specialist, taking into account the individual condition and needs of the patient. It is also important that massage is combined with other osteochondrosis treatment strategies, such as medication therapy, physiotherapy, and exercises, for maximum effectiveness.
Methods of osteochondrosis prevention
The prevention of osteochondrosis is a crucial aspect in avoiding or slowing down the development of this disease and its related symptoms. Prevention is comprehensive and includes several important factors that help maintain a healthy spine and joints. These factors include:
Physical activity
Regular physical activity is one of the most important aspects of osteochondrosis prevention. Exercises designed to strengthen the back, abdominal, and rib cage muscles help maintain proper spinal support and reduce pressure on the intervertebral discs. This also includes stretching and flexibility exercises, which help maintain a range of motion and reduce the risk of injuries.
Ergonomic work environment
Prolonged sitting, especially in an improper posture, can increase pressure on the spine and contribute to the development of osteochondrosis. It is important that the workspace is ergonomic, with proper sitting posture, computer monitor height, and accessibility to necessary tools.
Weight control
Being overweight is one of the factors that increase pressure on spinal discs and joints. Healthy eating and regular physical activity can help maintain an optimal body weight.
Healthy eating
A balanced diet rich in calcium and vitamin D is important for bone and joint health. This includes dairy products, fish, greens, and sunlight as primary sources of vitamin D.
Water consumption
Adequate water intake is important because intervertebral discs are largely composed of water. Dehydration can cause discs to dry out and become prone to injuries.
Posture correction
Proper posture, both sitting and standing, is important to prevent excessive pressure on the spine. Various exercises and activities, such as yoga or Pilates, can help maintain proper posture.
Adequate rest
Good sleep and adequate rest are important for spinal health. While sleeping, the body recovers, and this includes the renewal of spinal discs.
Quitting smoking
Smoking not only reduces circulation but also worsens the metabolism of intervertebral discs, which can contribute to disc degeneration.
Professional advice
Regular consultations with physiotherapists or chiropractors can help identify and correct issues that may cause or worsen osteochondrosis symptoms.
Learning and awareness
Understanding the risk factors for osteochondrosis and knowing how to reduce them are important aspects of prevention. This includes health and safety training at the workplace and independent information seeking.
By paying attention to these aspects of prevention and regularly applying them, it is possible to reduce the risk of osteochondrosis or slow down the progression of the disease. However, it should be emphasized that no method of prevention can completely prevent this disease, especially if there are other risk factors, such as genetics.

Information sources:
- World Health Organization (WHO)
- National Institutes of Health (NIH)
- National Institute of Arthritis and Musculoskeletal and Skin Diseases
- Mayo Clinic and Cleveland Clinic
# osteochondrozė