
Polycystic ovary syndrome (PCS) is one of the most common endocrine diseases in women, which directly affects reproduction and many other areas. Defined as a combination of hyperandrogenism and ovulation disorders, polycystic ovary syndrome (PCS) causes a range of symptoms that can include irregular menstrual cycles, excessive hair growth in unusual places (hirsutism), skin problems such as acne, and even infertility.
Too much androgen (so-called "male" hormones) can cause many small cysts to form on the ovaries, which can be seen on ultrasound. In addition, polycystic ovary syndrome is associated with a higher risk of cardiovascular disease, type 2 diabetes, and syndrome X (metabolic syndrome).
The exact etiology of PKS is complex and still not fully understood. It can be a genetic disease in which heredity plays an important role, but it can also be influenced by environmental factors, including diet and lifestyle. Polycystic ovary syndrome is associated with increased insulin resistance, when the body cannot respond to insulin properly, which can increase blood sugar and increase androgen production.
What are the causes of polycystic ovary syndrome?
Although polycystic ovary syndrome is one of the most common endocrine diseases in women, its causes are not fully understood. However, there are several important factors that can contribute to the development of PCOS.
Genetic predisposition: There is research showing that polycystic ovary syndrome may be hereditary. Women whose mothers or sisters have PCOS are more likely to have the syndrome as well. However, it is still not known which specific combination of genes can cause PKS.
Hyperinsulinemia and insulin resistance: Many, but not all, women with PCOS have insulin resistance, meaning their bodies cannot use insulin effectively. This causes hyperinsulinemia, when the body produces too much insulin. Elevated insulin levels can stimulate the ovaries to produce too much androgen, causing the symptoms of polycystic ovary syndrome.
Increased levels of androgens: Androgens are "male" hormones that are present in small amounts in women. However, women with PCOS have excess androgens, which can cause irregular menstrual cycles, hair growth in unusual places (hirsutism), hair loss, and other symptoms.
Weight gain and obesity: Weight gain and obesity can increase the risk of polycystic ovary syndrome. In addition, obesity can increase the symptoms of insulin resistance, which can lead to increased symptoms of PKS.
Inflammation: Research suggests that polycystic ovary syndrome may be associated with increased inflammation in the body. Inflammation can stimulate the ovaries to produce androgens, which can lead to symptoms of PCOS.
More research is still needed to better understand the etiology of PKS. In any case, polycystic ovary syndrome is a multifactorial disease in which both genetic and environmental factors play an important role.

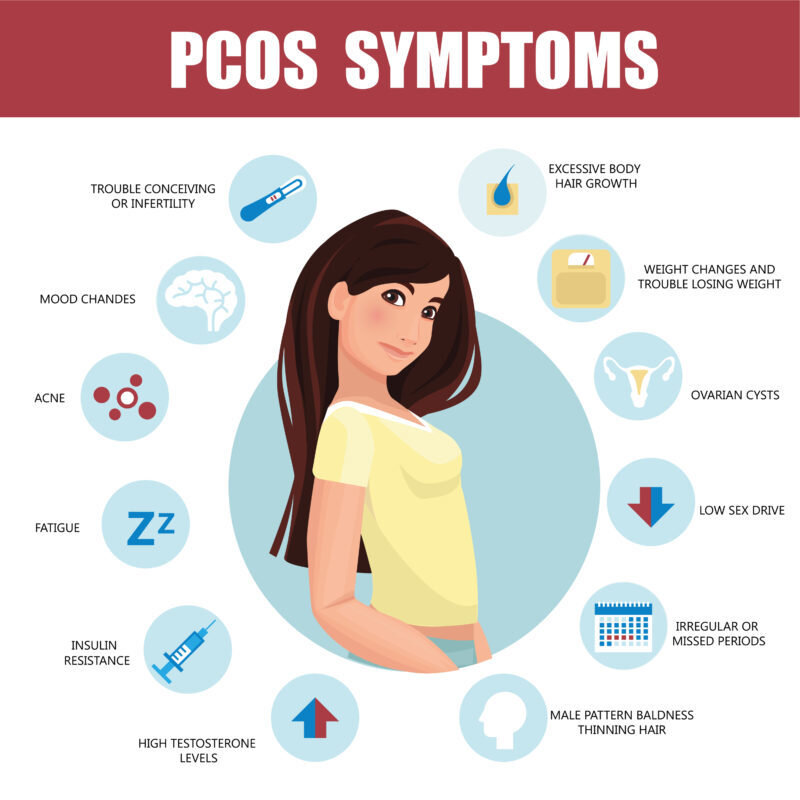
Symptoms
The symptoms of polycystic ovary syndrome are very varied and different between women, which makes this syndrome complex and often difficult to diagnose. Symptoms may begin in adolescence and continue throughout the reproductive years, but they can occur at any age. Here are the main symptoms of PCOS:
Irregular Menstrual Cycles: This is one of the most common symptoms. Some women may have long and unpredictable cycles, others may have fewer than 8 cycles a year or may stop altogether (amenorrhea).
Hirsutism: Hirsutism is the abnormal growth of male pattern hair in women, such as facial, chest and back hair growth. It is associated with increased levels of male hormones called androgens.
Skin rashes: Many women with PCOS experience skin problems, including acne and sebum production.
Weight gain and obesity: Polycystic ovary syndrome is closely related to overweight and obesity, especially when fat accumulates in the abdominal area.
Ovarian cysts: These cysts are small follicles that form in the ovaries. They can be detected by ultrasound, but many women with PCOS have no symptoms of cysts.
Thinning of scalp or hair loss: This is another symptom of hyperandrogenism that can occur due to PCOS.
Infertility: Polycystic ovary syndrome can lead to infertility due to irregular ovulation or absence of ovulation.
Insulin resistance and type 2 diabetes: Polycystic ovary syndrome can lead to insulin resistance, which can increase the risk of type 2 diabetes due to impaired insulin action.
Increased risk of cardiovascular disease: Metabolic disturbances associated with PKS may increase the risk of cardiovascular disease.
Mood disorders: Polycystic ovary syndrome can also cause emotional problems, including depression and anxiety.
These symptoms can be very different and range from mild to severe. Women who experience these symptoms are advised to seek medical attention.
How is polycystic ovary syndrome diagnosed?
Diagnosing PCOS can be difficult because its symptoms can vary widely and can sometimes be confused with other conditions. Doctors usually use the so-called "Rotterdam Criteria System" to diagnose PCOS, which requires at least two of the following three conditions to be present:
Irregular menstrual cycle or absence of ovulation, often manifested as irregular periods or longer than 35 days, or less than 8 menstrual cycles per year.
Clinical or laboratory signs of androgen excess, such as hirsutism (unpredictable growth of facial or body hair), hair loss, acne, or laboratory tests indicate elevated androgen levels in the blood.
Ovarian ultrasound imaging shows polycystic ovaries, the definition of which can vary between different doctors, but usually means that the ovary contains 12 or more small follicles (2-9 mm in size) or the ovary has a volume greater than 10 ml.
Before making a diagnosis of PCOS, it is important to perform a differential diagnosis and rule out other conditions that may cause similar symptoms. These may include hypothyroidism, hyperprolactinemia, Cushing's syndrome, androgen-producing tumors, and others.
In addition, your doctor may want to do additional blood tests to check for insulin resistance, cholesterol, and triglyceride levels to identify risk factors for cardiovascular disease and type 2 diabetes, which are often associated with polycystic ovary syndrome.
It is worth noting that the diagnosis of PKS is based on symptoms and clinical signs, not a specific test. This means that the diagnosis may vary between different doctors and clinics, and may require consistent medical examinations and follow-up.
Treatment
Although there is no cure for polycystic ovary syndrome, its symptoms can be managed, which usually improves the patient's quality of life. Treatment of PCOS usually depends on the patient's individual symptoms, lifestyle and pregnancy plans. Your doctor may recommend several different treatment strategies:
Lifestyle changes: This is the first and very important part of treating PCOS. This may include changes in diet and physical activity aimed at weight loss (if needed) and reducing insulin resistance. Studies show that even a 5-10% weight loss can improve symptoms of PCOS and increase fertility.
Hormonal contraceptives: Using oral contraceptives can help regulate menstruation, reduce androgen levels, and control symptoms such as hirsutism and acne.
Antidiabetic drugs: Metformin, an antidiabetic drug, can improve insulin resistance, help regulate menstruation, and reduce symptoms of PCOS.
Infertility treatment: Medications to stimulate ovulation, such as clomiphene or letrozole, may be recommended for women who want to get pregnant. Sometimes artificial insemination may also be recommended.
Androgen blockers: Medicines such as spironolactone or finasteride can help control hirsutism and hair loss. In addition, local methods of hair removal can be used.
Surgical treatment: In some cases, when other treatment strategies do not work, a surgery called ovarian perforation may be performed to stimulate ovulation. However, this procedure is not the first choice and is only recommended for certain patients.
All of these treatments can be used alone or in combination, depending on the patient's individual symptoms and needs. It is important to consult with your doctor for an appropriate treatment plan.
Prevalence
Most often, PKS is diagnosed in 6-10% of women of reproductive age, but this number may vary in different regions and between different ethnic groups.
Although PCOS is most commonly diagnosed in women of reproductive age, it can also occur in adolescence, when girls start menstruating. In addition, symptoms of PCOS may persist after menopause.
It is important to mention that many women with PCOS may be undiagnosed. Studies show that up to 70% of women with PCOS may be undiagnosed. This means that the real prevalence of PKS may be higher than official statistics indicate.
Early detection and effective management of PCOS is essential to ensure the best health outcomes. It requires ongoing medical care and an individualized approach based on each woman's specific symptoms and needs.
Polycystic ovary syndrome is an important public health issue, and more research and education continue to be needed to improve understanding, detection, and treatment of PCOS.
Sources of information:
Azziz R, Carmina E, Dewailly D, et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91(2):456–488.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25.
Franks S. Polycystic ovary syndrome. N Engl J Med. 1995;333(13):853–861.
Vink JM, Sadrzadeh S, Lambalk CB, Boomsma DI. Heritability of polycystic ovary syndrome in a Dutch twin-family study. J Clin Endocrinol Metab. 2006;91(6):2100–2104.
Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. 2012;33(6):981–1030.
Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO. The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab. 2004;89(6):2745–2749.
The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19(1):41–47.
Teede HJ, Misso ML, Costello MF, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602–1618.
Legro RS, Arslanian SA, Ehrmann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4565–4592.
# policistinių kiaušidžių sindromas
